The field of nanotechnology has revolutionized many areas of science, and medicine is no exception.
Nanomedicine is an interdisciplinary field that involves the application of nanotechnology to healthcare, with the aim of improving diagnosis, treatment, and prevention of diseases.
It involves the design, synthesis, characterization, and application of materials at the nanoscale level or nano-sized particles for medical purposes.
Definition of Nanomedicine
Nanomedicine refers to the use of nanoparticles or other nano-sized materials for medical applications. These tiny particles can be engineered to have specific properties, such as high reactivity or affinity for certain tissues or cells in the body. This allows them to be used as diagnostic tools or drug delivery vehicles that can target specific areas in the body with precision.
Importance of Nanomedicine in Healthcare

Nanomedicine has tremendous potential to revolutionize healthcare by providing more effective and targeted treatments with fewer side effects than traditional therapies. By using nanoparticles that are designed to target specific cells or tissues in the body, it is possible to deliver drugs directly to diseased cells while leaving healthy cells unharmed. This targeted approach holds great promise for treating diseases such as cancer without damaging surrounding healthy tissue.
In addition, nanomedicine can also be used for disease diagnosis by developing highly sensitive biosensors that detect small molecules and proteins associated with various diseases. These biosensors can provide real-time monitoring of disease progression and allow for early intervention before symptoms appear.
Historical Background of Nanomedicine

The concept of using nanotechnology in medicine was first proposed by physicist Richard Feynman in 1959.
However, it wasn’t until 1986 that Eric Drexler published a book called “Engines of Creation” that popularized the idea of nanotechnology as a way to revolutionize medicine. Since then, there has been a rapid growth in the field of nanomedicine, with numerous applications being developed for disease diagnosis and treatment.
The Science Behind Nanomedicine

Properties of Nanoparticles
Nanoparticles are very small particles that are typically less than 100 nanometers in size.
They can be composed of various materials, including metals, ceramics, and polymers.
Properties such as size, shape, surface area, and surface charge can significantly affect the behavior of nanoparticles in the body.
For example, particles with a larger surface area relative to their volume have more opportunities to interact with biological molecules and cells. Similarly, particles with a positive or negative charge can adhere to cell membranes or other surfaces more readily than neutral particles.
Types of Nanoparticles Used in Medicine
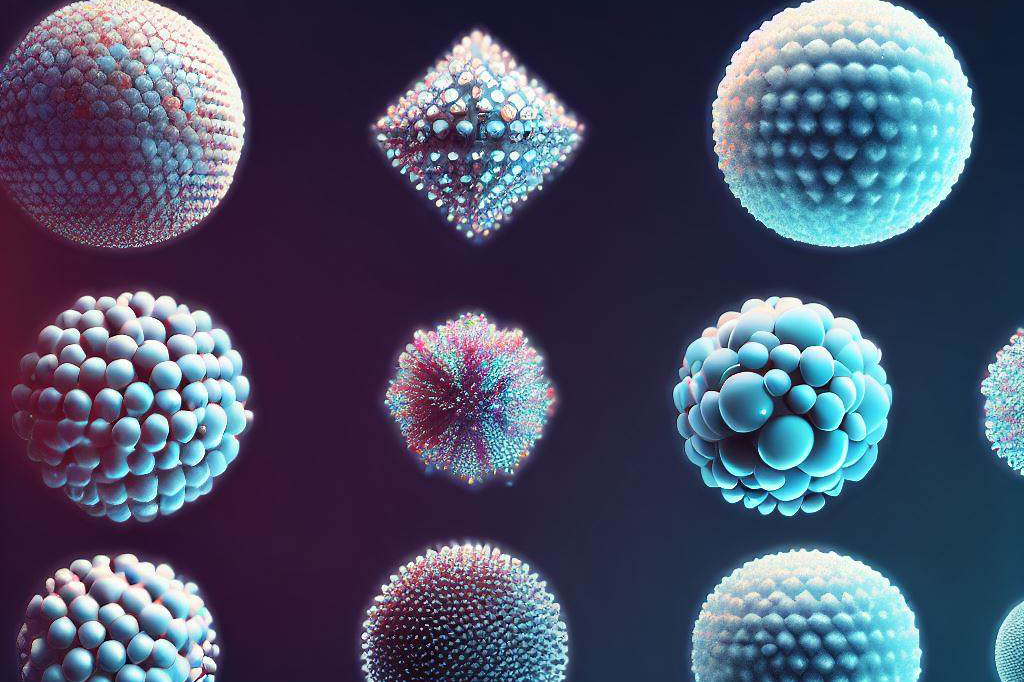
There are many types of nanoparticles used in medicine for a variety of applications. Some examples include
- liposomes,
- dendrimers,
- carbon nanotubes,
- metal nanoparticles (such as gold),
- and magnetic nanoparticles (such as iron oxide).
Each type has unique properties that make it suitable for different applications.
For example, liposomes are often used as drug delivery vehicles because they can encapsulate hydrophobic molecules inside their lipid bilayer structure. Dendrimers are highly branched polymeric structures that can be tailored to bind specific molecules or target specific cells.
How Nanoparticles Work in the Body
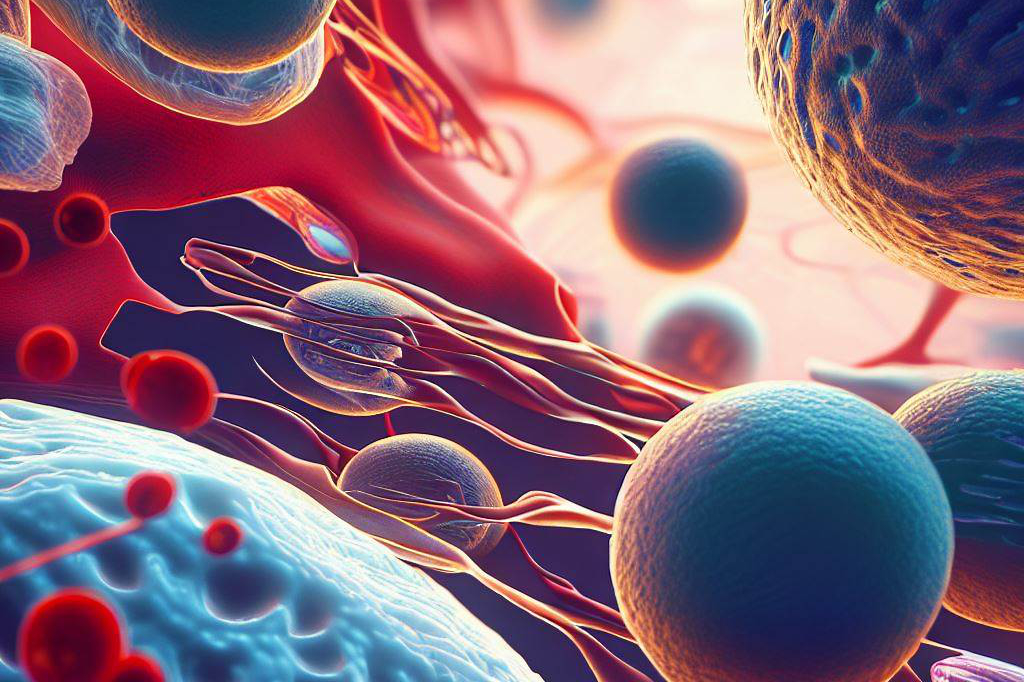
When tiny particles known as nanoparticles get into our bodies through eating, breathing, or injections, they interact with our body fluids and tissues. This interaction can make these particles stick together (aggregation) or get coated with specific proteins (opsonization) that make our immune system recognize and eliminate them. Our body disposes of these particles through natural waste processes or stores them in the liver.
Nanoparticles can also affect different parts of our cells, such as proteins, enzymes, and the genetic materials, DNA and RNA. This can change how genes work and increase how much our cells take in these particles. The amount taken up by the cells heavily depends on the particles’ size, shape, the functional groups on their surface, and how electrically charged their surface is, among other things.
The movement and distribution of nanoparticles in our body (pharmacokinetics and biodistribution) depend on what they’re made of, their size, and any modifications made to their surface. By altering these nanoparticles, we can make them focus on certain cells or tissues, help deliver medicines more effectively, or improve the clarity of medical images for diagnosis. Knowing how nanoparticles work and how they affect our bodies is key to developing useful nanomedicine.
Different types of nanoparticles have unique features that can be tweaked for specific medical uses. Furthermore, by using methods that make the most of these nanoparticle features, we can make them work better in detecting and treating diseases.
Applications of Nanomedicine
Nanomedicine has opened up a vast array of possibilities in the field of healthcare. There are numerous applications for nanotechnology in medicine, including disease diagnosis, drug delivery systems, and regenerative medicine. The following sections will discuss these applications in more detail.
Disease Diagnosis
One of the most significant applications of nanomedicine is in disease diagnosis. Nanoparticles have unique optical and electronic properties that make them ideal for use as diagnostic tools.
For example, gold nanoparticles can be engineered to emit light when they come into contact with specific molecules or cells. This property can be used to detect cancer cells in the body.
Additionally, nanoparticles can be functionalized with targeting moieties such as antibodies or aptamers that recognize specific biomarkers associated with various diseases. By detecting these biomarkers, nanoparticles can provide early detection and accurate diagnoses of diseases like cancer, Alzheimer’s disease, and cardiovascular diseases.
Drug Delivery Systems
Nanoparticles are also being used as drug delivery systems due to their small size, which allows them to penetrate deeper into tissues. They can also be functionalized with targeting moieties such as peptides or antibodies that recognize specific receptors on target cells, which improves their efficacy and reduces off-target toxicity.
Liposomes are one example of nanoparticle-based drug delivery system currently employed in clinical practice for chemotherapeutic drugs delivery by taking advantage of the tumor’s enhanced permeability and retention (EPR) effect. Liposomes encapsulate drugs within their hydrophobic core, and once administered, they accumulate preferentially at tumor sites while avoiding healthy tissue, thereby increasing efficacy while reducing toxicity.
Regenerative Medicine
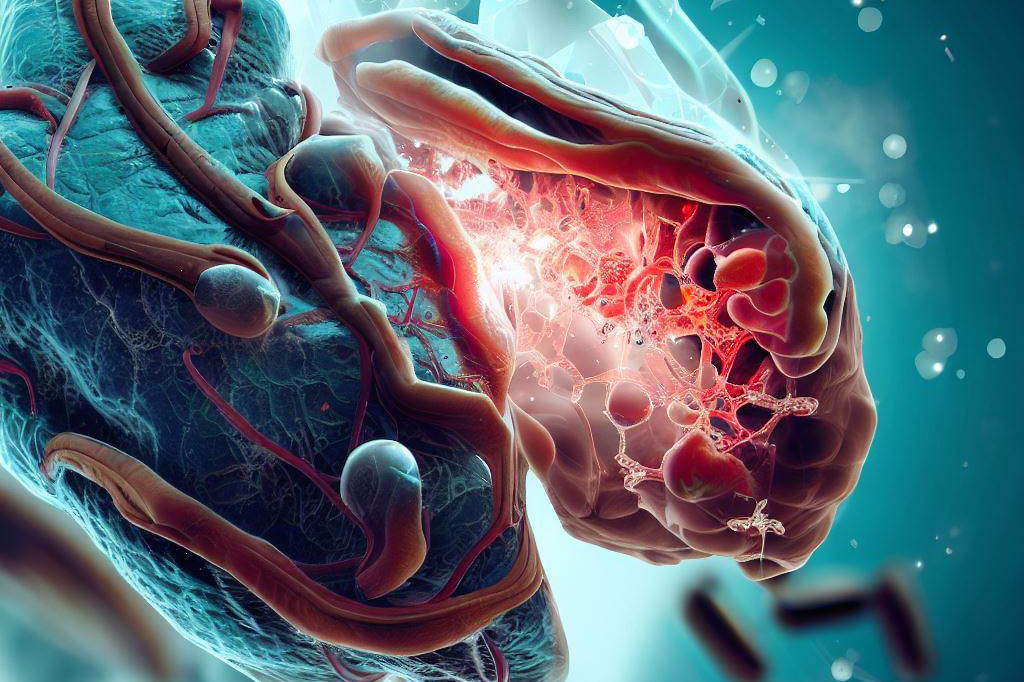
Regenerative medicine is another emerging application of nanotechnology, involving the use of nanoparticles as scaffolds or carriers for tissue engineering purposes or delivering growth factors necessary for tissue regeneration. Nanoparticles can be engineered to mimic the extracellular matrix, the natural environment for cells.
This helps in directing cell behavior and promoting tissue regeneration. Moreover, nanoparticles can also act as carriers for the delivery of regenerative medicine products like gene-therapy vectors that provide new genetic instructions to cells aiding in tissue repair.
In addition, nanoparticle-based strategies can be used to improve the efficacy of stem cell therapy by enhancing their homing and engraftment in target areas. Nanomedicine has brought about exciting possibilities in healthcare today.
From disease diagnosis to drug delivery systems and regenerative medicine, nanoparticles have opened up a new frontier for medical practitioners.
Advantages and Challenges of Using Nanoparticles in Medicine

Advantages
Nanoparticles have emerged as promising tools in medicine due to their unique properties, including their small size, high surface area, and ability to penetrate biological barriers. These features enable nanomedicine to target specific cells or tissues while minimizing damage to healthy cells. This targeted delivery reduces the toxicity of the drug on healthy tissue and increases efficacy.
1) Targeted Delivery
Nanoparticles can be engineered to deliver drugs directly to the site of action. This targeted delivery can be achieved by functionalizing nanoparticles with specific ligands that recognize receptors on cell surfaces. By utilizing this approach, drugs can be delivered directly to diseased cells while avoiding healthy ones, leading to increased efficacy with reduced side effects.
2) Increased Efficacy and Safety
The small size of nanoparticles allows them to penetrate biological barriers such as cell membranes or the blood-brain barrier, which are often a significant challenge for traditional drug delivery approaches. In addition, nanoparticles can increase the solubility and stability of poorly soluble drugs, leading to higher bioavailability and reduced toxicity.
3) Reduced Side Effects and Toxicity
The use of nanomedicine has the potential for reducing systemic side-effects that arise from conventional methods like oral administration, wherein a large amount of drug is given at once. By targeting specific regions or organs in the body using nanoparticles, there is a reduction in undesirable side effects seen with traditional medicines, which are administered via IV or orally.
Challenges
The development and implementation of nanomedicines face several challenges that limit their widespread adoption in clinical practice. These include regulatory issues, safety concerns, cost implications, and manufacturing challenges.
1) Regulatory Issues and Safety Concerns
The safety of nanomedicine is a topic of increasing concern as there are still many unknowns about the potential long-term effects on human health. Regulatory agencies such as the Food and Drug Administration (FDA) are tasked with evaluating the safety and efficacy of new drug delivery systems, including those that utilize nanoparticles. The lack of standardization between countries in regulation also hinders progress in this field.
2) Cost Implications
The cost implications surrounding the development and production of nanomedicines can be significant. Given their unique properties, nanoparticles often require specialized manufacturing processes that can be expensive to implement. Additionally, incorporating nanoparticles into existing drug formulations may require additional studies to test their effectiveness, which adds to the cost burden.
3) Manufacturing Challenges
The manufacturing of nanomedicine presents several challenges, such as reproducibility , scalability, and stability.
Several complex technologies are required for creating these nanoparticles, including microfluidics based synthesis, which makes it difficult to handle at scale or requires complexity in formulation optimization, leading to batch-to-batch variability . Additionally, stability issues like aggregation or degradation pose a challenge during long term storage, which requires proper measures at each step of production.
While nanomedicine holds great promise for revolutionizing healthcare and drug delivery due to its unique properties, several challenges must be overcome before widespread adoption can occur. Addressing these concerns through interdisciplinary approaches involving physicists, chemists, and biologists will ensure that these innovative technologies become a routine part of clinical practice, improving treatment outcomes for patients worldwide.
Future Directions for Research on Nanomedicine

Nanomedicine is an emerging field that holds immense potential in healthcare and drug delivery. As research continues to advance, future directions for nanomedicine include the development of new nanoparticles, enhanced imaging techniques, and more efficient drug delivery systems. One promising area of research involves the use of nanotechnology-based approaches for cancer treatment.
Nanotechnology-based Approaches to Cancer Treatment: A New Hope
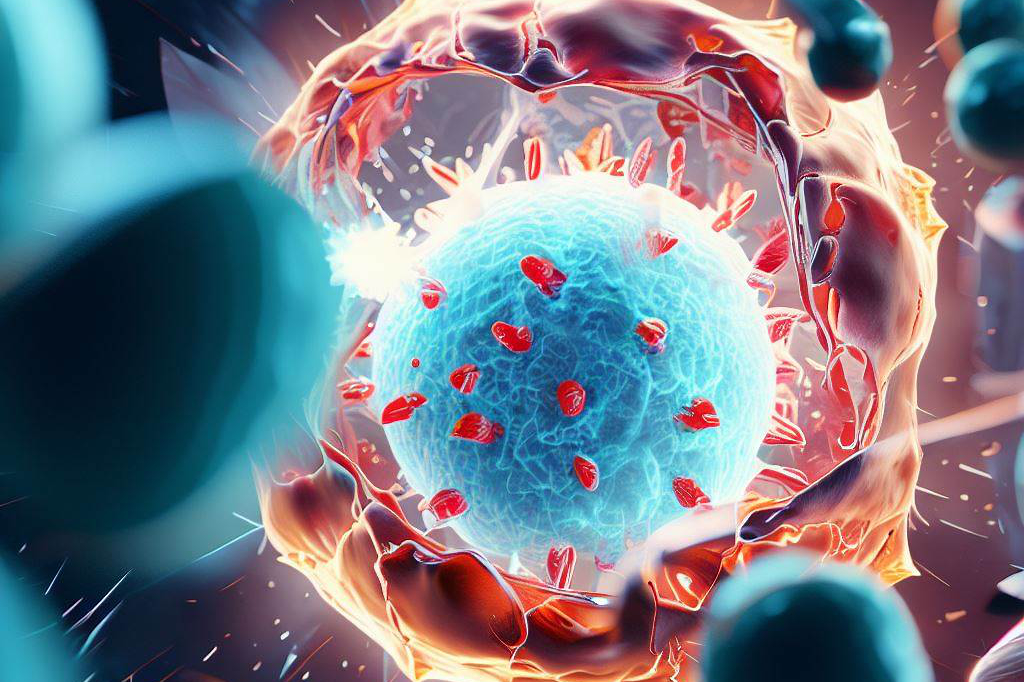
Cancer is a complex disease that requires innovative and targeted treatments. Nanoparticles have unique properties that make them ideal candidates for delivering drugs directly to cancer cells without harming healthy cells.
Researchers are exploring various strategies for using nanoparticles in the fight against cancer, including using them as carriers for chemotherapy drugs or as photothermal agents that can destroy cancer cells with heat. One promising approach is the use of multifunctional nanoparticles that can both detect and treat cancer.
These particles can carry a payload of drugs while simultaneously targeting specific cancer cells through their surface receptors or by binding to certain biomolecules found in tumors. Such approaches offer hope not only in treating cancers with poor prognoses but also in avoiding unwanted side-effects from conventional cytotoxic drugs.
Nanorobotics for Drug Delivery: Transforming Patient Care
The use of nanorobots could revolutionize drug delivery by increasing efficiency, reducing toxicity, and improving patient outcomes. Nanorobots are tiny devices that can be programmed to perform specific tasks, such as delivering drugs precisely where needed in the body or activating immune responses against tumor cells.
These devices could also help overcome some of the challenges associated with conventional drug delivery methods, such as poor bioavailability or rapid clearance from circulation. While still in the early stages of development, this exciting technology offers tremendous potential benefits to patients suffering from a wide range of diseases.
Nanobiosensors for Real-time Disease Monitoring: The Future of Healthcare
Real-time disease monitoring is critical for optimizing patient care and improving outcomes. Nanobiosensors offer a promising solution for monitoring disease progression in real-time through the detection of specific biomarkers or other molecular signatures. These devices can be designed to detect minute changes in the body, allowing for early intervention and treatment.
They could also be used to monitor concentrations of drugs or other therapeutic agents in the body, ensuring that patients receive optimal dosages without encountering adverse effects. The development of nanobiosensors holds enormous potential to transform healthcare by providing more precise and tailored treatments to individual patients.
Future directions for research on nanomedicine hold great promise as we continue to develop new technologies and approaches that can revolutionize healthcare and drug delivery. From cancer treatment to real-time disease monitoring, this exciting field offers tremendous opportunities for improving patient outcomes and transforming healthcare as we know it today.
Final Thoughts

Nanomedicine is rapidly advancing and holds great potential for revolutionizing healthcare and drug delivery. Through targeted delivery of drugs, nanomedicine has the ability to increase efficacy, reduce toxicity and side effects, and bring forth more personalized medicine.
The advantages of this emerging field are clear; however, there are also challenges that need to be addressed. Regulatory issues, manufacturing challenges, and cost implications must be overcome to ensure the widespread adoption of nanomedicine.

C M, a seasoned editor, journalist, and consultant, is deeply fascinated by the convergence of technology, space, and the future of humanity.
With a particular interest in transhumanism, futurology, and the philosophical and ethical dimensions of these domains, C M serves as the lead contributor to TranscendSphere and SpaceSpotlight.
When not penning insightful articles on these rapidly evolving fields, C M indulges in their love for podcasts and books, proudly embracing their status as a ‘Happy Nerd Extraordinaire!’